As the SARS-CoV-2 virus evolves, so too does the pathology of COVID. Now classed as a vascular disease, COVID infection can cause multi-system dysfunction involving the lungs, heart, kidneys, liver, blood, and brain.
What should we expect each time we catch COVID, and what are the lingering effects of Post-COVID Syndrome? From brain fog to COVID toes, here are the most common symptoms and how the immune system responds.
How Does SARS-CoV-2 Attack Cells?
Before we get into symptoms, let's look at the virus close-up. How does it spread and what the devil is it doing in our cells?
A COVID infection produces trillions of viral particles in the airways. Just 1ml of saliva contains more than 2 billion viral particles. Talking for five minutes, or coughing once, produces up to 3,000 respiratory droplets. The spread is uncontrollable.
Only a hundred or so viral particles need via the nose, mouth, or eyes to trigger an infection. Then the virus hones in on your cells, hijacking our tiny biological factories to create countless clones of itself. This is only possible because we share a genetic code. It's evidence that we're distantly related to the viruses that infect us.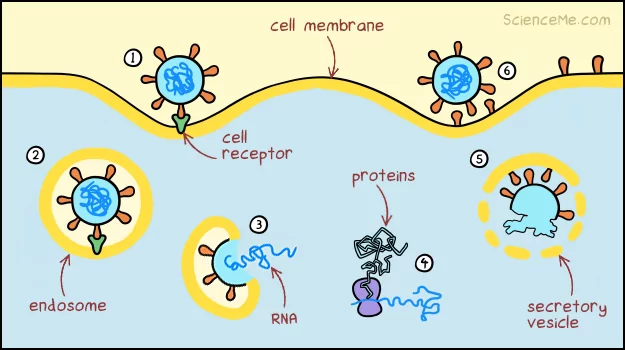
How coronaviruses replicate in cells.
The viral clones go on to infect more cells, causing the rate of infection to scale exponentially. Welcome to the incubation period of COVID-19. If this kind of biology has you salivating, check out my award-winning* post, How Does DNA Work?
*Awards issued by myself—to myself. The after party was amazing. The after party went on to win dozens of After Party Awards, which were also issued by me.
How Does The Immune System Fight COVID?
After a period of covert infiltration, the growing viral load triggers an immune response involving a network of specialist cells.
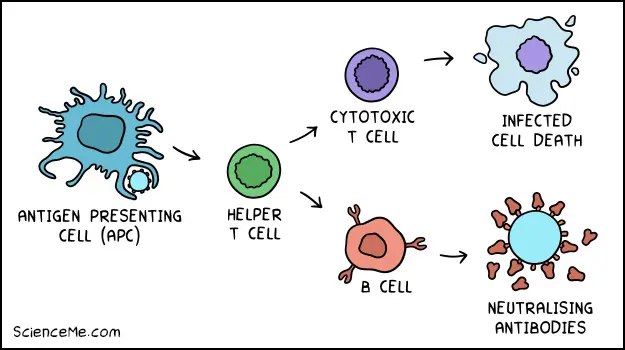
The adaptive immune system is a complex response involving Antigen Presenting Cells, helper T cells, cytotoxic T cells, B cells, and others.
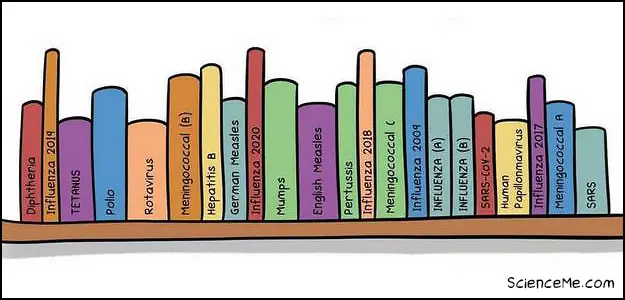
This adaptive immune response also creates memory B cells, allowing us to remember viruses and release tailored antibodies faster on subsequent encounters. It's like a personal pathogenic library that we stock up from birth.
Adaptive immunity evolved in vertebrates around 500 million years ago in our co-evolution with viruses.
If you're naïve to SARS-CoV-2, it takes the adaptive immune system 2-14 days to produce customised antibodies, and this latency is what allows COVID to make a mess of your insides.
The Early Symptoms of COVID
The first symptoms can actually be blamed on your innate immune response which is a generalised, fast-acting reaction to pathogens. During a COVID infection, your body tries to flush viral particles from the upper airways which causes:
- Coughing
- Mucus
- Sneezing
It turns out you have several orifices from which you can evacuate the virus. This is why some people experience:
- Nausea
- Vomiting
- Diarrhoea
When the virus attacks cells in the nose and throat, your immune system retaliates with the release of cytokines and chemokines. This results in inflammation which causes:
- Sore throat
- Hoarse voice
- Muscle aches
- Headache
- Brain fog
- Fatigue
- Blood clots
Cranking up your body temperature also helps those specialist immune cells recognise invading pathogens. This is why you get:
- Fever
- Chills
So what does COVID do to your body directly? As the virus replicates, it damages cells in the airways which soon results in:
- Loss of smell
- Shortness of breath
So you've got a fever, you're coughing, and you're fatigued. Life's not fair. But your immune system is fighting trillions of viral invaders right now. In a few days, your body will regain the upper hand and you'll feel much better. Or not.
Serious COVID Symptoms
If your body is unable to mount a decent immune response, you'll get a serious cases of COVID. Now we see the full force of the virus. Early COVID variants, including Wuhan and Delta, target the lungs aggressively. This reduces oxygen saturation and causes:
- Difficulty breathing
- Chest pain or pressure
- Confusion
- Drowsiness
- Pale skin and lips
These symptoms tend to begin after 5-8 days of moderate symptoms, indicating the virus has well and truly infiltrated the lower respiratory tract.
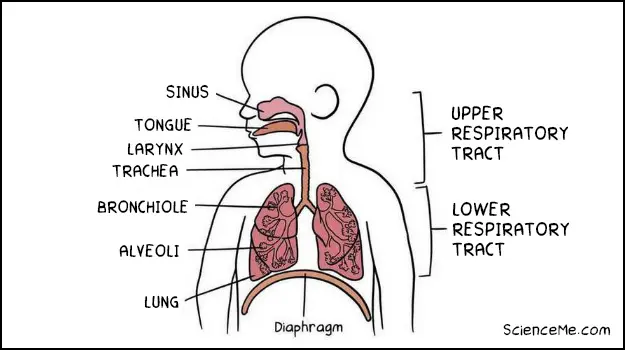
The upper and lower respiratory tract.
A viral infection in the lungs can lead to pneumonia which is inflammation of the lungs. The cells that make up the tiny air sacs degrade, filling up with fluid and pus from the surrounding blood vessels. This is what disrupts the vital oxygen supply.
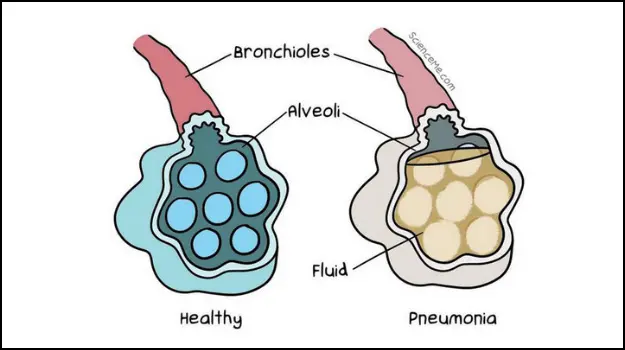
Pneumonia can seriously damage alveoli in the lungs.
While we can usually make a full recovery from pneumonia, COVID-induced pneumonia is different. It can cause severe injury to both lungs that can affect breathing permanently.
Patients with COVID pneumonia are at serious risk of Acute Respiratory Distress Syndrome, which causes a life-threatening lack of oxygen.
Early in the pandemic, ARDS affected 33% of all hospitalised COVID patients.
The condition marked by an excessive amount of fluid in the lungs. It prevents the 500 million alveoli from exchanging oxygen with carbon dioxide in the bloodstream. ARDS can catastrophically limit oxygen supply to the vital organs, such that up to 90% of COVID deaths are caused by ARDS.
Why Does COVID Cause Blood Clots?
The immune system responds to infection with inflammation, which in turn triggers blood clotting. This makes sense in the context of injury: if you open up your knee, inflammation calls up immune defences and clotting to close the wound.
But a systemic COVID infection causes excessive clotting. Small and large blood clots can lodge in the brain, heart, lungs, and legs.
COVID toes is the appearance of swollen red toes due to small blood clots triggered by COVID. Around one-third of hospitalised COVID patients have them.
If you have pain or swelling in one leg, it could be a sign of a large blood clot that needs immediate medical attention. Large blood clots can be fatal.
Long COVID Symptoms
Long COVID describes a vast array of symptoms that persist for more than 12 weeks after a COVID infection:
- Extreme fatigue
- Shortness of breath
- Heart palpitations
- Chest pain or tightness
- Loss of smell or taste
- Joint pain
- Brain fog
- Tremors
That's just the shortlist. One study identified 200 long COVID symptoms, affecting 10 different organ systems. Also known as Post-COVID Syndrome, it can occur after mild, moderate, and severe COVID infections alike.
Long COVID is likely the result of organ damage, or perhaps a persistent inflammatory or autoimmune response. For instance, 60% of COVID survivors have heart inflammation, which can cause shortness of breath, rapid heart rate, and palpitations.
Disturbingly, around 15% of people who've had COVID go on to develop long term neurological symptoms. This leads us to our next big question.
What Does COVID Do To Your Brain?
For some time, doctors had to assume that blood clots, inflammation, and cell death in the brain were side effects of the immune system dealing with COVID. Without evidence, it was simply too presumptuous to say that SARS-CoV-2 crosses the blood-brain barrier (BBB).
But after two years, German researchers found strong evidence that the blood-brain barrier is dysregulated by COVID infection. They say the virus enters the brain and wrecks havoc from within.
How? One possible entry route is the olfactory mucosa. The cells at the top of your nasal chambers are loaded with ACE2 receptors which act like docking sites for the virus. These cells provide an uninterrupted path directly to the brain.
This explains how COVID can create so many neurological problems:
- Stroke
- Encephalitis
- Haemorrhage
- Memory loss
- Confusion
- Psychosis
Indeed, COVID autopsies have found blood clots and severe damage to tissues in the lower brain stem (which controls heart rate and breathing) as well as the hippocampus (involved in learning and memory).
The developing brain may be especially vulnerable to COVID. Although children are far less likely to suffer from severe infection, a study of 1,700 hospitalised children showed neurological symptoms at a rate of 8%, rising to 22% in children with underlying brain conditions. Their symptoms included:
- Encephalopathy
- Stroke
- CNS infection
- Guillain-Barre syndrome
- Cerebral oedema
While most of these children had transient symptoms and survived, a minority still suffered life-threatening conditions from COVID.
The good news is that COVID is a mild or asymptomatic illness in the majority of children. There's at least one good explanation for this: testosterone increases the number of ACE2 receptors on cells. Children, and indeed, women, have less testosterone than men and are thus less susceptible to severe COVID infection.
Final Thoughts
Fortunately, the Omicron variant eased up on pathogenicity. But there's no guarantee the next variant will be as mild. Spanish Flu likely evolved into a deadlier variant before it became endemic, while Ebola has become more pathogenic over time.
Science continues to hone in on the widescale effects of the SARS-CoV-2 virus. While doctors are familiar with the individual symptoms of COVID, the novel disease mechanisms pose entirely new riddles.
Why is COVID pneumonia so aggressive? How does COVID cause brain injury? Are the symptoms of long COVID permanent? There's still a great deal to investigate before we fully understand what COVID does to your body.
Written and illustrated by Becky Casale. If you like this article, please share it with your friends. If you don't like it, why not torment your enemies by sharing it with them? While you're at it, subscribe to my email list and I'll send more science articles to your future self.